As the days grow shorter and the vibrant colors of autumn fade into the gray of winter, many people report feeling a dip in energy or a shift in mood. This is often colloquially referred to as the “winter blues.” However, for a significant portion of the population, these seasonal shifts trigger a more severe, clinical form of depression known as Seasonal Affective Disorder (SAD).
At Formal Psychology, we believe in understanding the biological and psychological underpinnings of our moods. This guide explores what SAD is, why it happens, and the evidence-based strategies used to treat it.
What is Seasonal Affective Disorder?
Seasonal Affective Disorder is not considered a separate disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Instead, it is classified as a specifier for Major Depressive Disorder (MDD) with a seasonal pattern.
This means that individuals with SAD experience episodes of major depression that recur at specific times of the year. While it is most commonly associated with the fall and winter months (“Winter-Pattern SAD”), a less common form occurs during the spring and summer (“Summer-Pattern SAD”).
Who is at Risk?
SAD is estimated to affect millions of adults worldwide. Key risk factors include:
- Gender: SAD is diagnosed four times more often in women than in men.
- Geography: People living far north or south of the equator (where winter daylight hours are shortest) are at higher risk.
- Family History: Individuals with a family history of SAD or other forms of depression are more susceptible.
- Age: Young adults are more likely to experience SAD than older adults.
Symptoms: More Than Just “Feeling Down”
Symptoms of SAD typically start mild and become more severe as the season progresses. Because SAD is a form of major depression, the core symptoms remain consistent, but the specific manifestations often depend on the season.
General Symptoms of Major Depression
Regardless of the season, individuals may experience:
- Persistent feelings of sadness or hopelessness.
- Loss of interest in activities once enjoyed.
- Changes in appetite or weight.
- Difficulty concentrating.
- Thoughts of death or suicide.
Winter-Pattern SAD (Fall/Winter)
This is the most common presentation and is often characterized by “hibernation-like” symptoms:
- Oversleeping (Hypersomnia): Difficulty waking up in the morning and excessive daytime sleepiness.
- Appetite Changes: Specifically a craving for foods high in carbohydrates (bread, pasta, sugar).
- Weight Gain: A direct result of increased carb intake and reduced activity.
- Low Energy: Feeling “heavy” or having leaden paralysis (heavy feeling in arms or legs).
- Social Withdrawal: A strong desire to isolate and “hibernate.”
Summer-Pattern SAD (Spring/Summer)
Though rarer, summer depression presents distinct, often agitated symptoms:
- Insomnia: Difficulty falling or staying asleep.
- Poor Appetite: Leading to unintentional weight loss.
- Agitation and Anxiety: Feeling restless or on edge.
- Irritability: Increased incidents of violent or aggressive behavior are sometimes noted.
The Psychology and Biology: What Causes SAD?
Researchers have not pinpointed a single cause for SAD, but it is widely believed to be a complex interplay of biological markers triggered by a lack of sunlight.
1. Circadian Rhythm Disruption
Your body has an internal biological clock (circadian rhythm) that regulates sleep, mood, and hormones. Reduced sunlight in fall and winter can disrupt this clock, causing it to fall out of sync with your daily schedule, leading to feelings of depression.
2. Serotonin Levels
Serotonin is a brain chemical (neurotransmitter) that affects mood. Reduced sunlight can cause a drop in serotonin, a chemical that affects mood. This deficit may trigger depression.
3. Melatonin Production
Darkness triggers the production of melatonin, the hormone that makes you sleep. In winter, the longer hours of darkness may cause the body to overproduce melatonin, leaving individuals with SAD feeling lethargic and sleepy.
Diagnosis and Professional Treatment
Diagnosing SAD requires a thorough evaluation by a mental health professional. To meet the criteria, an individual must have experienced depression during specific seasons for at least two consecutive years, with the seasonal episodes significantly outweighing non-seasonal episodes.
Once diagnosed, treatment is often highly effective.
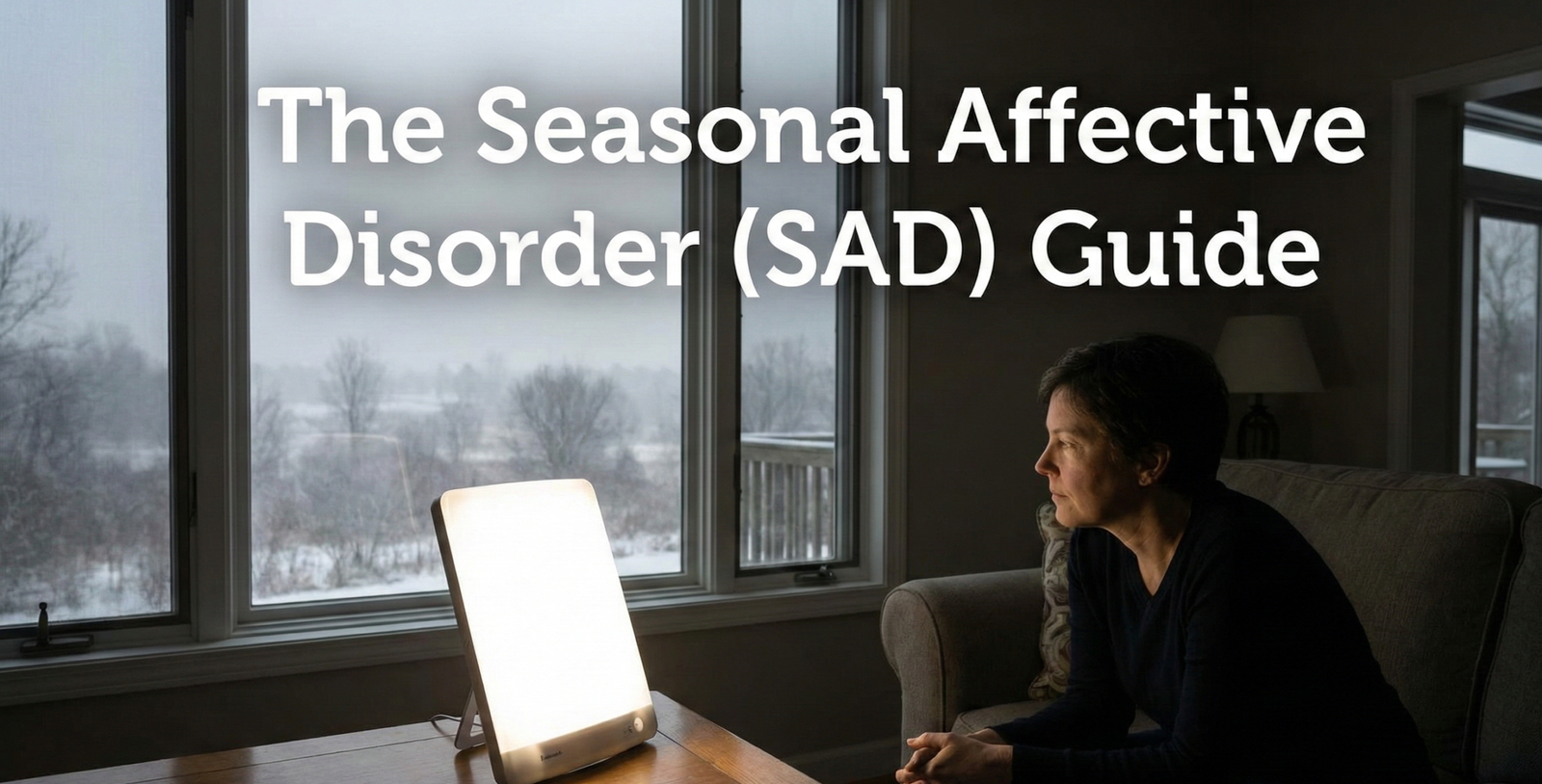
1. Light Therapy (Phototherapy)
This is the first-line treatment for Fall/Winter SAD. It involves sitting in front of a specialized light therapy box for 20–60 minutes shortly after waking up.
- How it works: The box mimics outdoor light (without harmful UV rays), triggering a chemical change in the brain that lifts mood.
- Intensity: Standard boxes provide 10,000 lux of light.
2. Psychotherapy (CBT-SAD)
Cognitive Behavioral Therapy (CBT) has been adapted specifically for SAD. It focuses on:
- Identifying and changing negative thoughts about the season (e.g., “I hate winter, I can’t do anything”).
- Behavioral Activation: Scheduling pleasant, engaging activities (indoors or outdoors) to combat the urge to hibernate.
3. Medication
Selective Serotonin Reuptake Inhibitors (SSRIs), such as antidepressants, are often prescribed to regulate serotonin levels. In some cases, doctors may recommend starting medication before symptoms begin each year as a preventative measure.
4. Vitamin D
While studies are mixed, many people with SAD have low Vitamin D levels due to lack of sun exposure. Supplementation is often recommended to support general health and bone strength, which may adjacently support mood.
Coping Strategies: Managing SAD Daily
Beyond clinical treatment, lifestyle adjustments play a crucial role in managing Seasonal Affective Disorder.
- Soak Up the Sun: Open blinds, trim tree branches that block sunlight, and sit closer to bright windows. Even on cloudy days, outdoor light is brighter than indoor light.
- Get Moving: Regular exercise is a potent depression fighter. It helps reduce anxiety and improve sleep. Outdoor exercise serves a dual purpose by adding sunlight exposure.
- Stick to a Schedule: Waking up and going to sleep at the same time every day helps regulate your circadian rhythm.
- Socialize: Resist the urge to isolate. Make plans with friends or family to keep your mind active and engaged.
Conclusion
Seasonal Affective Disorder is a real, treatable condition. It is not a sign of weakness or an inability to handle the weather; it is a biological response to environmental changes. If you notice distinct shifts in your mood as the seasons turn, we encourage you to speak with a healthcare provider. With the right combination of light therapy, talk therapy, and self-care, you can find stability and joy regardless of the time of year.